Can Alzheimer's Be Stopped?
Season 43 Episode 8 | 52m 51sVideo has Closed Captions
Join investigators as they untangle the cause of Alzheimer’s and race to develop a cure.
Alzheimer’s disease strikes at the core of what makes us human: our capacity to think, to love, and to remember. The disease ravages the minds of over 40 million victims worldwide, and it is one of the greatest medical mysteries of our time. Join investigators as they gather clues and attempt to reconstruct the molecular chain of events that ultimately leads to dementia.
National Corporate funding for NOVA is provided by Carlisle Companies. Major funding for NOVA is provided by the NOVA Science Trust, the Corporation for Public Broadcasting, and PBS viewers.
Can Alzheimer's Be Stopped?
Season 43 Episode 8 | 52m 51sVideo has Closed Captions
Alzheimer’s disease strikes at the core of what makes us human: our capacity to think, to love, and to remember. The disease ravages the minds of over 40 million victims worldwide, and it is one of the greatest medical mysteries of our time. Join investigators as they gather clues and attempt to reconstruct the molecular chain of events that ultimately leads to dementia.
How to Watch NOVA
NOVA is available to stream on pbs.org and the free PBS App, available on iPhone, Apple TV, Android TV, Android smartphones, Amazon Fire TV, Amazon Fire Tablet, Roku, Samsung Smart TV, and Vizio.
Buy Now

NOVA Labs
NOVA Labs is a free digital platform that engages teens and lifelong learners in games and interactives that foster authentic scientific exploration. Participants take part in real-world investigations by visualizing, analyzing, and playing with the same data that scientists use.Providing Support for PBS.org
Learn Moreabout PBS online sponsorshipTONY ESTRELLA: When I talk to her about what she's got coming up, she can no longer trust, "Is that the right date?
"Was that the right time?
I don't remember that."
You know, they'll be lots of cross-outs.
You can't make heads or tails out of it."
The calendar ends up looking like an abstracted, two-dimensional version of the interior of the mind.
You know, what happens when you're forgetting and you can't trust what you remember?
(sighs) We're in this week here.
I know.
What day are we at?
NARRATOR: Tony Estrella's mother Donna has Alzheimer's, a disease that attacks the brain, destroying one's ability to think and function.
ESTRELLA: On some level, you know, Alzheimer's is a kind of death in life, when your mom or your dad no longer recognizes their son or daughter.
The person is no longer there, and yet they are.
Deal with that.
Come on in.
Okey-dokey.
NARRATOR: Donna is taking an experimental drug, hoping to stave off dementia.
The companies testing Alzheimer's drugs have their own hopes.
An effective treatment will not only help patients, but bring in billions of dollars.
We're seeing dozens and dozens of pharma companies and biotech companies around the world developing therapies to either treat, prevent, or slow down this disease.
Huge investments are at stake.
A lot of time and effort's at stake.
We know that this is an extremely risky endeavor.
Because one clinical trial after another has failed.
NARRATOR: From the barrios of Colombia to cities across the world, new drugs are being tested.
As everyone waits for results and uncertainty rules, one thing is clear: Alzheimer's is an epidemic.
This isn't a cris that's gonna happen years from now.
We're in the throes of this crisis right now.
NARRATOR: Up next on NOVA, "Can Alzheimer's Be Stopped?"
Major funding for NOVA is provided by the following... NARRATOR: The memory lapses were troubling: forgotten appointments, misplaced objects, irretrievable names.
Reporter Greg O'Brien dismissed them as the result of too much stress and normal aging.
GREG O'BRIEN: I was experiencing horrific short term memory loss.
I wasn't recognizing people that I knew.
I wasn't recognizing places.
And I just felt if I ignored it, it would go away.
NARRATOR: Then a bike crash resulting in a concussion and brain scans unmasked the problem.
Alzheimer's, a progressive, incurable brain disease, and the most common type of dementia.
Greg was not just losing his keys, but also his memory.
At age 64, he's chronicling the progression of his disease.
One of his first priorities is to shatter the stereotype of Alzheimer's.
O'BRIEN: Alzheimer's is not just your grandfather's disease.
There are scores and scores of people who are in the early stages of Alzheimer's right now and may not even know it, because this is a disease that can take 20 years or more to run its course.
Tell me how many children you have.
(sighs) I'm sorry, I'm...
It's just not there?
It's just not coming up.
What is the date today?
I don't know.
Where are you originally from?
I think... that's a toughie.
O'BRIEN: Alzheimer's is not only my story, it could be your story, or the story of a relative or a close friend.
(thunder clap) What's this?
That is a, um... NARRATOR: The human toll is staggering.
It starts with a "B."
NARRATOR: Over 40 million people are afflicted with Alzheimer's, including five million Americans.
And the numbers are rising.
How about this thing, what's that?
REISA SPERLING: Baby boomers are coming up fast, and it's estimated that 10,000 individuals in the U.S. turn age 65 every single day.
And age 65 is where it really ramps up quickly the likelihood of developing Alzheimer's disease.
So we're projecting that it's gonna be ten million in another 20 years.
It's going to grow to epidemic proportions.
It has the potential for bankrupting the entire medical system.
But I also have to think of the human side of this.
It's hard to think of anything that's more sad than a person who's done so much in their life and accumulated a lifetime of memories and to have all of that lost in the their last few years.
Oh, that's my youngest daughter.
No... SPERLING: And the inability to form new memories and remember things that are happening to them every day gets lost progressively in Alzheimer's disease.
And as you can imagine, that's terrifying.
NARRATOR: The urgent need to find a treatment for Alzheimer's is driving a global race.
Virtually every large drug maker is competing.
One place where the stakes are high is at Genentech, a biotech company in South San Francisco.
Like many of its rivals, Genentech is developing a treatment to prevent or slow Alzheimer's.
But it faces stiff competition, with some 20 drugs in trials in the U.S. alone.
The probability of failure is high.
Less than one percent of Alzheimer's drugs tested have been approved, and none of them can stop the disease.
Medical director Carole Ho believes that's about to change.
15 years ago, when I was starting to study Alzheimer's Disease, I did not think that in my lifetime I would ever see a therapy that would really benefit patients.
Given the acceleration over the last ten to 15 years in understanding the disease, and now having very targeted therapies that go directly after what we think the source of the disease is, I'm incredibly hopeful.
NARRATOR: Neurobiologist Ryan Watts agrees.
RYAN WATTS: I think we know so much that it's a great place to really put in the intellectual power to try to figure out how to treat this disease.
"Cure" is always a strong word, but I think what I imagine is that we develop a treatment that can then become a prevention.
NARRATOR: The search for a treatment is decades old, the progress slow and incremental.
ERIC SIEMERS: I know that a lot of people wonder, "How have you gone "through 25 years without having a medication successfully make it to the marketplace?"
And I think the only real answer to that is we were learning every step along the way.
NARRATOR: The disease was first identified in 1906 by psychiatrist Alois Alzheimer.
During an autopsy, he examined the brain of Auguste Deter, who had entered his mental hospital delusional and confused.
Before her death, she told him, "I have lost myself."
Alzheimer rejected the notion of madness, suspecting a physical illness had killed her.
A sliver of stained tissue magnified hundreds of times proved he was right.
WATTS: I think it was very striking, what he must have seen, looking at these big clumps of protein, known as plaques.
In fact, they were everywhere, riddling the brain.
He also observed tangles, which you can see here, inside the neurons.
NARRATOR: Alzheimer sketched the features of the disease that would bear his name.
Plaques and tangles clearly distinguished it from other dementias.
But were they a direct cause of the disease?
(clock bells chiming) To find the answers, scientists searched for rare families where Alzheimer's was passed from generation to generation.
Pa, pa. NARRATOR: On the outskirts of Medellín, Colombia, Ramiro tends to his father Nelson.
For eight years, he has been sick with dementia and unable to work as a driver.
RAMIRO (translated): Six months ago, he was able to walk.
Slowly, but he could stand on his own.
Now he no longer recognizes me.
He doesn't know my name.
He doesn't speak.
He doesn't understand anything.
He's a total infant.
NARRATOR: Nelson is part of a family where dementia starts unusually early, around age 45.
Dr. Francisco Lopera, a Medellín neurologist, has treated the family for decades, starting with Nelson's mother.
(translated): What I found most shocking was her age-- that she was a young person with Alzheimer's-type dementia.
I was also struck by the fact that several of her relatives had the same history of disease.
From the time we identified the first family, we knew we were facing something very important.
NARRATOR: Lopera would soon discover other families with the same pattern of illness.
In a nearby town, Salome tends to her aunt, Yolanda, ill for over a decade.
Salome has watched dementia tear apart her family.
(translated): I started to realize that it was something that went back to my great-grandmother.
That's when I started to get scared.
I realized my mother could get sick.
In addition to worrying about my mom, I really worry that I might get the disease.
That's why I don't want to have children.
NARRATOR: Lopera asked psychologist Lucía Madrigal to help him construct genealogies of the families, suspecting an inherited disease.
But the families had their own explanation.
(translated): They believed they had been cursed, charmed, or given some kind of magic potion.
And people make up stories to explain and bring meaning to what they're going through.
So they hung on to this idea of witchcraft, the myths and beliefs of the region.
NARRATOR: As Lopera followed a trail of dementia across Colombia, his work caught the attention of Ken Kosik, an Alzheimer's researcher.
KOSIK: From the moment I saw this piece of paper on which he had just mapped out a small piece of this family, it was clear it was genetic because if they had one parent affected, they were facing a 50/50 chance of either getting it or not getting it in these families.
And the families were large enough to say that.
There wasn't just, like, two people.
It was 15 people, and you can see that about half would get it.
That is a clear-cut signature of a genetic condition.
NARRATOR: Lopera was convinced a rare form of dementia determined by genes plagued the region.
But were the afflicted families related?
To find out, he visited local parishes, combing through birth, death, and marriage records.
As he traced their ancestry, an extended family of 5,000 members emerged.
Those with dementia descended from a Spanish conquistador.
To find out if their illness was Alzheimer's disease, Lopera examined the brain of a victim.
When he compared it to a healthy brain, it was abnormally small.
He sent it to Kosik.
KOSIK: And we went right into my lab, cut the brain, stained it, and were able to see that the brain was absolutely full of plaques and tangles-- the diagnostic signature of Alzheimer's disease.
NARRATOR: Lopera's team had found the largest extended Alzheimer's family in the world.
Clearly, there was a genetic explanation.
But what gene was involved?
And did it implicate either plaques or tangles as the cause of Alzheimer's?
In the 1980s, attention focused on plaques after scientists discovered they were made from a protein called amyloid beta.
Little is known about its role in the brain.
Normally, fragments of amyloid are cleared away.
But in Alzheimer's, they accumulate like garbage, forming plaques.
Could a faulty gene be the problem?
JOHN HARDY: Everybody's got a copy of the amyloid gene, and that gene gave us geneticists something to work with, something we could look for mutations in.
NARRATOR: John Hardy and Alison Goate studied the gene in British families who, like the Colombians, had a history of Alzheimer's.
Like all genes in our DNA, the one responsible for the amyloid protein is made up of four chemical bases abbreviated by the letters A, T, C and G. Goate probed the gene in afflicted families, hunting for incorrect letters, known as mutations.
GOATE: This is detective work.
We were reading the DNA sequence by hand and looking for the one spelling mistake that was causing disease in the families.
A, T, T, C, C... NARRATOR: Among the 3,000 letters making up the gene, Goate finally found a mutation.
In the DNA of one family, everyone with Alzheimer's had the same mistake: a "C" replaced by a "T." GOATE: We could see, looking across the gel, "This one's affected, yes, they carry the variant.
"This one's unaffected, they don't carry it."
So we were pumped, I dare say.
We definitely found something.
You know, you're looking at it and you're saying, "Wow!"
NARRATOR: The mutation appeared to cause amyloid to clump into plaques.
HARDY: And we immediately realized that amyloid was central to the disease process, and what researchers should do is focus on reducing amyloid in the brain.
NARRATOR: Hardy and other scientists put forth a bold idea: amyloid plaques trigger the cascade of destruction, including tangles, that causes Alzheimer's.
Soon, other mutations were found that also implicated plaques.
The one afflicting the Colombians was pinpointed by Alison Goate, working with Lopera's team.
Now, the families confronted a stark reality: anyone who had inherited this mutation was destined to get Alzheimer's.
There was no escape.
(translated): At first, it was very difficult to tell them they had a disease.
It's real, and every child has the same odds.
Suddenly, we were opening Pandora's box.
I used to ask if we were doing the right thing.
The box had been opened, but where was the hope?
NARRATOR: But on the horizon, there was hope.
The knowledge gleaned from these families was pushing the field forward.
Drug makers now had a target, and people at risk everywhere stood to benefit.
After years of research, Genentech, like many of its rivals, has developed a potential Alzheimer's drug.
It's designed to target amyloid, which makes up plaques.
WATTS: You look at a human brain, and they start to form these little clumps, or pieces of garbage.
We ask ourselves, number one, how can we stop the production?
And number two, how can we get rid of the existing garbage that's there?
That's the problem, and the solution arises from the tools that we have at hand, which are basically the body's own immune system.
NARRATOR: The drug is an antibody, similar to the ones found in our blood.
It binds to amyloid and signals immune cells to destroy it.
Many companies are testing similar antibodies, and some have run into serious problems.
Shehnaaz Suliman, who helps manage the testing, is well aware of the challenges.
We're all extremely hopeful, but also extremely nervous because the history of Alzheimer's drug development has been fraught with difficulty and failure.
Some drugs have caused brain swelling in patients who have been in clinical trials.
So that's a side effect that we will track very closely.
NARRATOR: The drug will be tested in a series of clinical trials, divided into three phases.
WATTS: So we ran a relatively large phase one clinical trial, and that was designed to test this question around safety.
And phase one indeed showed that the drug is not going to cause this swelling in the brain.
So that's a good start.
NARRATOR: The drug was ready for a phase two trial to determine its effectiveness and the best dose.
It would first be tested in the U.S. and Europe, not on the rare familial type of Alzheimer's, but on the most common form, where the cause is less clear.
The vast majority of Alzheimer's occurs after 60, and, yes, there you see genes playing a role.
But they don't guarantee the disease.
NARRATOR: Over 500 people sign up for the 18-month study, treating patients like Joanne with mild to moderate Alzheimer's disease.
Hi, Dr. Salloway.
How are you doing?
Good, how are you?
NARRATOR: Stephen Salloway oversees clinical trials at Butler Hospital in Providence, Rhode Islan SALLOWAY: The early stages of Alzheimer's disease if you have a good, stable living situation can be associated with a very good quality of life.
However, it's a progressive illness, and our goal for this trial is to see if we can actually slow the progression of the disease process itself.
NARRATOR: A third of the patients will get a high dose of the drug, a third will get a low dose, and the rest will get a harmless placebo.
The trial is a double-blinded study, meaning neither patients nor doctors will know who is getting the drug.
Inside knowledge or expectations could taint the results.
SULIMAN: If there's any kind of bias which occurs in the trial, the trial results could be null and void.
I'm going to start off with asking you, do you have trouble with your memory?
Yes.
NARRATOR: Patients like Bonnie are given cognitive tests similar to this one.
What is the date today?
I can't...
Okay, that's fine.
NARRATOR: People with mild to moderate Alzheimer's cannot answer many simple memory questions.
Now, I want you to listen carefully because I'm going to say three objects to you.
And when I'm finished, I'd like you to repeat those objects back to me.
Are you ready?
All right.
All right, here they are.
Apple, penny, table.
Apple, penny, table.
All right, now try to remember those because I'm going to ask you about them again in a little bit.
Now, spell the word "world" backwards.
L-R-O-W.
Okay.
Now, what were those three objects I had you remember?
All right, any guesses?
No.
NARRATOR: During the trial, patients getting the placebo are expected to decline, serving as a control group.
If Bonnie gets the drug, the hope is that her scores will stay the same or decline at a slower rate compared to untreated patients.
People don't realize that stability is a very good outcome for a progressive illness like Alzheimer's.
If there's no change over a year or 18 months, then it's a very good outcome.
NARRATOR: Bonnie is beginning to enter the moderate stage of Alzheimer's.
She has stopped working because she can't trust her memory.
BONNIE: I can't say it's good.
I have little bits and pieces that come together, and then I can figure out what's going on.
DAVID COLETTA: We do have selfish reasons for doing the study, let's face it.
I want her back.
I want her the way she was.
But if she could stay the way she is right now, I'd be happy.
I'll take what I can get.
I'll take it too.
Yeah.
NARRATOR: But the outcome of the trial hangs on key questions.
Will the drug stop plaques from forming in patients' brains?
And if it does, will this slow or halt dementia?
In Colombia, Genentech's drug will also be tested, but in a different type of trial.
Working with the Colombian families, scientists will try to prevent Alzheimer's from striking at all.
So this is truly a unique opportunity to intervene early and show that you can actually prevent the onset of symptoms.
TANZI: So if you're doing a prevention trial, this is the ideal population to use.
We know who's going to get the disease, guaranteed, and let's see if we can prevent it in them, and then you really know whether your drug, your treatment is working.
NARRATOR: To see if the drug can stop plaques from forming, scientists will rely on new advances in imaging.
Amyloid can now be tagged with radioactive chemicals so it appears in vivid color in brain scans.
Eric Reiman used the new imaging on the Colombian families and made a startling find.
REIMAN: By doing these studies in carriers of this Alzheimer's-causing gene versus non-carriers from the same family, we were able to detect these brain changes earlier than many people expected.
NARRATOR: The imaging captured a "silent period."
Plaques, seen in red and yellow, started accumulating in carriers around age 30 and peaked some ten years later, well before the onset of symptoms.
It was a revelation: plaques form long before dementia begins.
REIMAN: Indeed, we believe that everybody at risk for Alzheimer's disease begin to have the underlying biological changes two decades or more before the onset of symptoms.
Now, that may sound frightening, but that also provides a window of opportunity in which to intervene, to strike at the disease before the clinical symptoms ever begin.
NARRATOR: Reiman's work became the catalyst for launching the preventative trial in Colombia.
Ramiro wants to sign up, but he has concerns.
It's a five-year commitment, and no one has taken the experimental drug that long.
RAMIRO (translated): I was hesitant at first because when you're feeling well, when you don't feel anything, it's very hard to commit before you know whether or not you'll get Alzheimer's.
NARRATOR: Over the next several months, the families visit Dr. Lopera to learn more about the trial.
(translated): So why have you been invited here?
Because you're all members of a family at risk for a genetic disease.
NARRATOR: To enroll, everyone must be screened to be sure they have no cognitive impairment.
The trial includes people who have the mutated gene, as well as those who don't.
Half of the carriers will get the drug.
Everyone else gets the placebo.
And nobody will be told his or her genetic status.
I remember so clearly a case of a 24-year-old boy who I asked, "If we can tell you whether or not you have the disease, would you want to know?"
He said, "Yes, I want to know."
He said, "If I have that mutation..." And he did this.
He said, "I'll shoot myself."
Now, this kid is 24 years old.
He's got another 24 years until he, even if he has the mutation, would get the disease.
Lots of things are happening in that interval.
Genetic information is fire.
NARRATOR: For participants like Hugo, there are practical concerns.
One is taking time off from work for periodic brain scans.
HUGO (translated): I had this form for my boss to sign, giving me permission, and he said, "If you want to be a lab rat, go ahead."
But I just said thanks.
I don't fight with him.
Why?
I'm no rat.
It's an experiment they're doing, and it's for us, so I don't worry about it, because if they cure me, they'll cure my children.
NARRATOR: If Hugo carries the mutation, doctors expect to see plaques forming long before symptoms occur.
LOPERA (translated): And if he is a carrier and receives the drug, and if it's successful, at the end of the study, we hope to see that the first scan has a lot of amyloid, the second has less amyloid, and the third has much less, or is almost free of amyloid.
NARRATOR: Only independent experts will know if the drug is working.
Everyone else, including Genentech, will have to wait until 2020 for results.
TANZI: The drug company has to sit back and hope for the best while, essentially, the fate of the drug is in the hands of others who are running the trial and assessing the data.
So it's a long trial, very expensive, but likely to give you answers.
NARRATOR: Back in the U.S., Genentech's mild to moderate Alzheimer trial is ending.
I don't want you to move your head at all.
I'll do all the moving, okay?
NARRATOR: The scanning technique used in Colombia was too new to monitor everyone in this study.
Bonnie is part of a small group of patients getting their final scans.
She doesn't know if she's been taking the drug or the placebo.
But now that the trial is officially over, Bonnie and every patient can receive the drug for a period of time.
DAVID: At times, I think her memory's getting worse, and at times, I think it's leveled.
And, I mean, I can live with this, I mean, every day asking me what day it is.
He has no choice.
Exactly.
I'm hoping this study is working.
This would be a miracle, I mean, an absolute miracle.
NARRATOR: At Genentech, it's time to find out if their drug has helped patients with Alzheimer's.
The data from the trial will be revealed in a private meeting.
The event is called the "unblinding."
He's on the telephone.
There's so much human emotion tied up in this.
Did you sleep well last night?
No.
Everybody in a company is working so hard to develop these drugs.
Hey Robert, how are you?
I'm fine, how are you?
Good.
Good Monday?
Yep, did you sleep well last night?
I'm incredibly optimistic that we may see something that really will benefit people.
NARRATOR: Senior Vice President Sean Bohen knows success depends on the trial's design.
BOHEN: When you test a hypothesis in the clinic, a lot of it is dependent upon how you conduct the trial.
What do you measure?
How accurately and consistently do you measure it?
It takes a lot time and, frankly, money to get there.
NARRATOR: Bohen hopes the $350 million trial will lead to a big breakthrough.
But even a hint that the drug works in some patients will be considered a step forward.
The moment of truth.
BOHEN: If you took a poll of this team, this team I think feels pretty confident it will be positive.
Five, four, three, two, one.
I think it's going to be more complicated.
According to the atomic clock, it's 11:00.
NARRATOR: For now, only the core team will have access to the reams of information collected.
It will take months to analyze the details and find out if they're on the right track.
The results will be made public at an international Alzheimer's conference the following year.
As clinical trials forge ahead, millions of patients confront Alzheimer's relentless progression.
Greg O'Brien struggles with rapid mood swings.
O'BRIEN: You just feel like such a dumbass, you know?
And I know I'm not.
I'm not stupid, I just have a disease.
You know, I love my family, I love my friends, but I don't love myself so much anymore.
I don't love myself so much anymore.
CONOR O'BRIEN: I remember picking up his phone months ago when it was cracked.
My dad said he dropped it, but what he really did was he didn't know how to dial and he got mad and he threw it against the wall.
MARY CATHERINE O'BRIEN: If I thought his rage was part of his personality, how disturbing would that be?
And how angry would I be?
So when I see him upset and angry, I know that it's not him, it's the disease.
NARRATOR: Having watched his mother die from Alzheimer's, Greg knows what's coming.
O'BRIEN: You lose your self-esteem, but you don't want people to feel sorry for you.
So you fight back, you fight back, you fight back.
NARRATOR: While patients around the world wait for a treatment, scientists fighting Alzheimer's convene in Copenhagen, Denmark.
At the Europa Cafe, Sean Bohen and Carole Ho prepare themselves for a critical presentation.
Researchers from rival companies and universities are eager to hear if Genentech's drug worked.
The Genentech team already knows the answer.
Carole Ho recalls the roller coaster of events that led up to this moment.
So that day when the door closed, that was the first of actually two unblindings from our data, and this was the unblinding actually of the low dose.
JEFFREY CUMMINGS: In the low dose group, there's essentially no difference between the drug and the placebo.
NARRATOR: The low dose clearly failed, but what about the high dose?
CAROLE HO: So fast forward a few months after that, we then unblinded the high dose.
And now we had all the data, and all of a sudden, that lens was just opening up.
CUMMINGS: In the high dose group, there is a drug-placebo difference in the more mild patients.
NARRATOR: While mild patients on placebo declined as expected, those taking the high dose declined 35% less on cognitive tests.
When I saw the data, the first thing that came to my mind was just this overwhelming sense of relief that in the milder patients at the higher dose, we saw some signals that suggest we're having success.
That's incredibly promising for earlier stages of disease.
NARRATOR: But do the results warrant spending nearly a billion dollars on a large phase three trial for mild Alzheimer's patients?
After a few months, a decision is made to move forward.
And in Colombia, where they are intervening early, they will switch to a higher dose to give the preventive trial its best shot at success.
KOSIK: And, of course, the people here in Colombia are as mild as you can get.
They don't have symptoms yet.
So each trial stands on the shoulders of the previous one, allowing insights to proceed as everything in science does-- incrementally.
NARRATOR: In Cambridge, Massachusetts, a biotech company called Biogen set out to capitalize on the lessons of past trials.
Its scientists designed a selective phase one safety trial, hoping to get clear results.
Instead of treating moderate Alzheimer's, Biogen only enrolled patients like Donna, with mild or early stage disease.
And they scanned every patient to be sure they had plaques that their drug could target.
The results exceeded expectations.
It appeared that the more drug that was given, the more amyloid plaque was removed from the brain.
And the longer that person was on the drug, the more plaque was removed.
So we believe we have proof that our drug is getting into the brain and attacking the plaques and reducing them.
Having done that, the next step is really, does it matter?
Does that contribute to improvement in cognition?
Now, I'm going to show you a few common objects.
NARRATOR: Although the primary aim of the study was to test the drug's safety, Biogen also gathered cognitive data.
What is this?
Pacifier.
What is this?
Screwdriver.
And what is this?
That's a good question.
I don't know.
I know what it is, but... NARRATOR: With only 166 patients in the study, it was too small to draw definitive conclusions.
But a signal did emerge.
TANZI: And there, we saw that lowering amyloid in the brain of mild patients correlated with a slower decline in cognition, especially for the highest dose of the drug.
NARRATOR: In contrast to patients on placebo, those taking the high dose declined some 80% less on cognitive tests.
But there were side effects.
TANZI: Things like edema, or swelling in the brain.
So many of those patients had to drop out.
REISA SPERLING: So it's something we want to avoid because we have to make sure people don't develop any significant damage from the amyloid removal.
And, unfortunately, this side effect will limit how much of these antibodies we can give to people as we're trying to help their brains remove the amyloid.
NARRATOR: For Tony Estrella, the risk seems worth taking, especially if the trial leads to a successful drug for his mother.
Where is that arrow?
Can you tell me what that arrow is connecting?
It's connecting from 11 to 9.
Hm...
So you think you changed it from 11 to 9.
That's why you crossed out the nine.
I don't know.
ESTRELLA: You're looking for a lifeline of some kind, because it's unknown territory.
And so with that comes a certain amount of fear about what's going to happen to your mom.
And all of a sudden, you can't help but think about yourself as well.
And my grandfather had Alzheimer's as well.
And so you think about, "Well this isn't gonna stop here," which makes this trial so important.
NARRATOR: Betting that the side effects can be managed, Biogen is taking the gamble and jumping directly to phase three trials, treating thousands of patients.
AJAY VERMA: We are in the midst of testing a hypothesis that the world has been challenged to test.
We think this is a very viable target.
It may not be the only target.
And huge investments are at stake.
A lot of time and effort's at stake.
KOSIK: We're looking for a signal somewhere, a signal that would show that we're on the right track.
And in the last couple years, a small signal is beginning to emerge, suggesting that these antibody therapies may provide us with a treatment.
NARRATOR: The key to success appears to be giving these antibodies early.
Reisa Sperling thinks clearing plaques from the brains of baby boomers might avert an epidemic.
She's running a preventive trial for people at risk for ordinary Alzheimer's using a drug developed by Eli Lilly.
In past trials, it slowed memory loss 34% in mild Alzheimer's patients.
SPERLING: So this suggested to us that if we could go even ten years earlier in people who barely have any symptoms or no symptoms at all and slow cognitive decline by 30%, we could really prevent dementia in a large proportion of individuals.
Most of those people would die out ballroom dancing instead of in a nursing home.
So I didn't have a heart attack or anything?
(laughs) You are doing just fine.
Go ahead and sit up.
NARRATOR: Art Canter knows that scans have detected plaques in his brain.
He also fears his memory lapses may not be normal aging.
So he's joined the preventative trial.
ART CANTER: You can be the ostrich, you know, if you want to stick your head in the sand and just say, "Well, whatever happens, happens."
So yes, it's high stakes for all of us who are going through this whole process, but at the same time, there's the potential of what they might find in whether or not the meds will work.
NARRATOR: While preventing plaque buildup may keep Alzheimer's at bay, Sperling suspects this approach won't help everybody, especially as the disease advances and another culprit identified by Alois Alzheimer over a century ago, begins to wreak havoc: tangles.
It's been known that two different changes happen in the brain of people with Alzheimer's disease.
One is the build-up of amyloid into plaques, and the other is what we call tangles that accumulate inside the nerve cells.
NARRATOR: Tangles are made of a protein called tau, which help stabilize neurons and allows them to communicate.
Yet in Alzheimer's disease, tau is corrupted and twisted into tangles.
As tangles form and neurons die, the symptoms of dementia set in.
But why does tau go bad?
Insights are coming as new advances let scientists image and track tau in the brains of living patients.
SPERLING: So, the first thing we found when we started to look at tau scans is that almost everybody over the age of 65 or 70 has some tangle buildup very deep in the brain.
KEITH JOHNSON: Now, these are still normal people, but at a certain point in some individuals, the tau just is transformed.
It tangles.
It proliferates, it propagates into other places in the brain.
It just spreads like crazy.
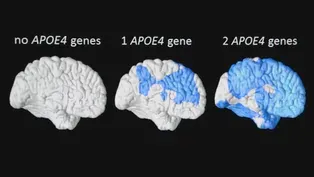
NARRATOR: And the reason becomes obvious when amyloid and tau scans from the same person are compared.
SPERLING: In Alzheimer's disease, people don't get tangles spreading throughout their brain unless they have amyloid.
So currently, we think that amyloid pulls the trigger and tau is the bullet that unfortunately kills the nerve cells.
And when that happens, now people begin to get demented.
So if we're gonna have a treatment, you can't ignore tau.
This is a complex disease that needs a multi-pronged attack.
TANZI: Now we're seeing the first drugs going into clinical trials to stop the tangles from spreading, but we don't know what problems they're going to see.
Coming up with the right therapy that's safe, gets into the brain, it's potent, hits the right target, this is part of drug discovery.
It's incredibly hard.
NARRATOR: As tau drugs enter testing, Genentech, Biogen, and Lilly await the results on their antibodies targeting amyloid.
Even if they slow dementia, they will not be silver bullets or help everyone.
Still, experts predict we may see the first drugs to treat the cause of Alzheimer's by 2020.
But progress also depends on getting people to join clinical trials.
It really is a very promising time for the field, and I think that's one thing that patients should keep in mind, is that if we can enroll these trials in half the time, we get the answers much, much sooner.
There's only one way out of this problem, and that's research.
And the research community is really active, and the insights are coming rapidly.
And that is where we're going to get an answer.
There we go.
NARRATOR: Bonnie can no longer be left alone.
Since her husband's sudden death, her daughter has moved back home to help.
After 16 years of illness, Yolanda passed away.
But many of her relatives have entered the preventive trial.
(translated): They want to find a way to break that chain, and they want a better future for their children.
It's the first time in 30 years they've had any hope.
NARRATOR: To prepare for his future, Greg is selling his Cape Cod home.
GREG O'BRIEN: Alzheimer's is like having a sliver of your brain shaved off every day.
And you get up the next day and you say to yourself, "Okay, where am I gonna be today?"
And it is scary.
I don't know what's going to happen, I don't know who's going to show up.
I've got to get it together.
And I don't know when that light in my brain's going to go off.
But I want society to take this disease, Alzheimer's, seriously.
This is hell on wheels, and it's racing right for us.
The great mammals are in trouble.ia Access Group at WGBH access.wgbh.org This NOVA program is available on DVD.
To order, visit shopPBS.org, or call 1-800-PLAY-PBS.
NOVA is also available fo r download on iTunes.
Inside the Mind of Alzheimer’s
Video has Closed Captions
Journalist Greg O'Brien gives a first-hand account of what it's like have Alzheimer's. (4m 23s)
Video has Closed Captions
Certain gene forms increase your risk of developing Alzheimer's. (2m 38s)
Providing Support for PBS.org
Learn Moreabout PBS online sponsorshipNational Corporate funding for NOVA is provided by Carlisle Companies. Major funding for NOVA is provided by the NOVA Science Trust, the Corporation for Public Broadcasting, and PBS viewers.