Addiction
Season 45 Episode 12 | 53m 45sVideo has Closed Captions
Discover how opioid addiction affects the brain and how treatments are saving lives.
Hear firsthand from individuals struggling with addiction and follow the cutting-edge work of doctors and scientists as they investigate why addiction is not a moral failing, but a chronic, treatable medical condition. Easy access to drugs like heroin, fentanyl, and even prescription medications like OxyContin has fueled an epidemic of addiction—the deadliest in U.S. history.
National corporate funding for NOVA is provided by Draper. Major funding for NOVA is provided by the David H. Koch Fund for Science, the Corporation for Public Broadcasting and PBS...
Addiction
Season 45 Episode 12 | 53m 45sVideo has Closed Captions
Hear firsthand from individuals struggling with addiction and follow the cutting-edge work of doctors and scientists as they investigate why addiction is not a moral failing, but a chronic, treatable medical condition. Easy access to drugs like heroin, fentanyl, and even prescription medications like OxyContin has fueled an epidemic of addiction—the deadliest in U.S. history.
How to Watch NOVA
NOVA is available to stream on pbs.org and the free PBS App, available on iPhone, Apple TV, Android TV, Android smartphones, Amazon Fire TV, Amazon Fire Tablet, Roku, Samsung Smart TV, and Vizio.
Buy Now

NOVA Labs
NOVA Labs is a free digital platform that engages teens and lifelong learners in games and interactives that foster authentic scientific exploration. Participants take part in real-world investigations by visualizing, analyzing, and playing with the same data that scientists use.Providing Support for PBS.org
Learn Moreabout PBS online sponsorship♪ ♪ NARRATOR: A devastating epidemic... KEN: We just didn't know what to do.
We just felt powerless.
A parents' worst nightmare, to find my kid not breathing.
JAMES WINNEFELD: He was always very good at telling us, "Mom and Dad, everything's going to be fine," but it wasn't.
NARRATOR: Addiction is ruining lives and ending them too soon.
(alarm blaring) Overdose is the number one cause of death for people under 50.
RAHUL GUPTA: We are racing against time.
We have the equivalent of a Boeing 737 crashing every single day.
NARRATOR: But what causes addiction?
ROBERT MALENKA: Individuals struggling with addiction are actually battling millions of years of evolution, because our brains are exquisitely evolved, to seek rewards.
It's those cravings, the inability to stop.
NARRATOR: A dangerous cocktail of biology and medicine made deadlier by a drug 100 times more potent than morphine.
DARWIN FISHER: Fentanyl is super toxic.
So you get a batch that comes on the street that's a little bit hot, and on those days, it's like, bam, somebody's going down.
Bam, somebody's going down.
Bam!
NARRATOR: But can new treatments offer hope?
LAURA KEHOE: We have extremely effective medications that are life-saving.
This is a very treatable illness.
ANNA LEMBKE: The solution to this is for us to embrace addiction as a disease, to bring it within the house of medicine.
FISHER: People recover from addiction.
Nobody is unreclaimable.
The only thing that you can't recover from is death.
NARRATOR: "Addiction," on "NOVA."
♪ ♪ Major funding for "NOVA" is provided by the following: ♪ ♪ NARRATOR: McDowell County, West Virginia, feels like a place left behind.
Yet its miners helped power America when coal was king.
Back then, the largest city, Welch, was a thriving community.
But as coal jobs vanished by the 1990s, the poverty rate in the county climbed to 38%.
Then investigators found that over a six-year period, drug companies had flooded the state with 780 million highly addictive pain pills.
(train horn blaring) (rumbling) JASEN EDWARDS: West Virginia was the perfect storm.
The whole state's dominated by one of the hardest and most dangerous jobs in the world.
Most of the old timers that work in the mines work with pain.
And then pain pills started flooding the community, and people that you used to know weren't the same people that they used to be.
I mean, it, it just... it ruined everything.
♪ ♪ NARRATOR: Jasen Edwards and his two brothers Scott and Mark, grew up in Sophia, West Virginia.
The town was near the Winding Gulf coal field.
Most of its residents were miners, including the Edwards family.
All three sons would struggle with pain pills.
Jasen got his first prescription after crushing his leg in a mining accident.
They cut my leg off the day after Christmas in 2008, and I was back underground mid-to-late February.
First day I went back to work, I had to crawl everywhere or ride everywhere I went, because my stump was still too swollen to put my prosthetic leg on.
A man hurts his back, if he is not back to work, they will replace him.
And I could not have supported my family on the disability.
NARRATOR: Soon, a few pills a day could no longer stop the pain.
(drill grinding) But Jasen could easily buy more by visiting doctors and showing his artificial leg.
JASEN: The first time I realized that I was in trouble is when I couldn't go to work, because I didn't have any pain pills.
And it wasn't because of how bad I was hurting, it was because of the sickness due to detoxing.
♪ ♪ NARRATOR: Jasen was addicted to a powerful opioid painkiller called OxyContin.
Opioids like OxyContin are chemically similar to morphine, found in the opium of the poppy plant.
They mimic the body's natural pain relievers, like endorphins, which bind to proteins, called receptors, calming pain and inducing euphoria.
Prolonged opioid use can alter the brain and lead to addiction, manifested by cravings and compulsive drug use despite negative consequences.
♪ ♪ As opioids were aggressively marketed, West Virginia soon had the highest rate of overdose deaths in the U.S., alarming health commissioner Dr. Rahul Gupta.
GUPTA: We were amongst the top states prescribing pain pills in the nation.
At the same time, people were losing their employment, they were also losing a way of life.
It spelled the perfect conditions under which addiction began to creep in.
(indistinct talking) ♪ ♪ NARRATOR: At Stanford University, psychiatrist Anna Lembke also feared Big Pharma's pressure on doctors was creating an epidemic.
When she got access to patients' prescriptions records, her suspicions were confirmed.
Many people abusing pain pills were getting them from doctors-- not drug dealers.
♪ ♪ I'll never forget when I first looked at the drug database for a patient of mine.
I mean, it was just glaringly obvious she'd been doctor shopping, you know, 1,600 pills, I think, in the span of a month.
And I think it's important to know that doctors were being sued if they did not do everything within their power to address a patient's pain.
So there was a serious problem going on here.
NARRATOR: Lembke was also seeing a new type of patient-- an "opioid refugee."
(dog barking) KEN: How's your chemistry class coming?
CASEY: It's fine.
What are you guys working on in there?
Compounds, chemical compounds, like iron... NARRATOR: Casey leads a protected life.
Her father Ken watched drugs destroy his brothers, so he moved his daughters out of the city and put them in private schools.
In her teens, Casey stayed busy with sports.
But she began having severe muscle cramps.
CASEY: I remember one game in particular, all of sudden I just started feeling really shaky and then everything just started hurting.
My legs and my arms just cramped up really tight.
She fell straight to the ground screaming in pain.
It took me and one of her coaches to pick her up, put her in our car, rush her out to Children's.
They did a million and one tests, and then they found, you know, an ovarian mass.
Well, an ovarian mass in a teen, that's scary.
So then that required more medical workup in order to discover that the mass was, in fact, benign, but by then, you know, she had a surgery, it had been removed, and through all of this, she received copious opioids.
♪ ♪ CASEY: Once I left the hospital, I noticed that I was still having a lot of pain, but it was nowhere near the surgery sites that they had operated on.
KEN: We couldn't even touch her, she was in so much pain.
She described it as it felt like her bones were being ripped out of her body.
Now, the pain she was experiencing was opioid withdrawal pain, but they didn't know.
So they whisk her back to the emergency room.
"What could this possibly be?
She's got terrible pain."
And, essentially, every single time the solution was, "Prescribe more opioids."
But after a while they didn't help as much anymore, so I started taking way too many.
LEMBKE: Until at one point an emergency room doctor realized she's addicted, and what was his reaction?
He basically went out and he shamed them.
And he's like, "Your daughter's addicted.
We never want to see her here again."
NARRATOR: Stunned, Ken drove home, with no idea of how to help his daughter.
Casey was now an opioid refugee, battling cravings and withdrawal on her own.
We just felt powerless.
And as a dad, I'm supposed to be her protector, and I just felt like I had, I had completely let her down, that...
I just didn't, I mean, I just didn't know what, what to do anymore.
♪ ♪ LEMBKE: There was implicit trust.
"If this medication were dangerous, "they would tell me.
"As long as we take it just as prescribed, everything is going to be okay."
And that is totally untrue.
Casey's a great example.
Now, given her family history of addiction, she probably had an underlying vulnerability, right?
But what made her addicted was the opioids that she received from her doctors.
NARRATOR: Addiction runs in families, and studies suggest that genes play a role in determining one's risk.
Addiction is a complex disorder, and as a complex disorder, there's not one addiction gene.
It's multiple genes and multiple other factors that interact with your genetics that increases risk.
NARRATOR: Over 90% of addiction cases start before age 21, when the brain is still forming.
For Jasen's brother Mark, it was a time of impulsive decisions.
MARK EDWARDS: I had no idea how dangerous pain medication would be.
I never woke up any day and said, "Man, I want to be an addict today."
And I asked myself, "How did you end up here?"
And I look back on my surroundings and everything that was around me.
People everywhere was, was doing this.
It was almost like there was nothing else in life.
♪ ♪ NARRATOR: As doctors prescribed fewer pain pills, drug cartels filled the void by selling heroin, an illegal opioid cheaper than OxyContin.
Overdose deaths climbed as heroin, long available in inner cities, turned up in rural communities.
♪ ♪ In a single year, more than 70,000 Americans died of an overdose.
Addiction is America's number one domestic issue today.
We have hospitals that are overwhelmed with people who need help.
We have a prison system that is filled with people who actually need treatment.
We have judges that are often seeing more people with mental diseases than a psychiatrist-- or a primary care physician like me-- sees in a day.
The entire fabric of our society is being destroyed, as a result of addiction.
♪ ♪ NARRATOR: Addiction is often viewed as a moral failing-- stigmatized by words like "clean," "dirty," "abuser," "addict."
But scientists now know it's a disorder that occurs as the brain changes in response to drugs.
MALENKA: Individuals struggling with addiction are actually battling millions of years of evolution, because our brains are exquisitely evolved to seek rewards, to seek reinforcement wherever and whenever we can.
♪ ♪ NARRATOR: To understand how reward shapes behavior, Robert Malenka simulates a famous experiment.
A mouse is attached to a fiber optic cable and placed in a cage with two holes.
♪ ♪ When the mouse explores the hole on the right, a flash of light sparks a feeling of pleasure in its brain.
At the other hole, nothing happens.
Yep, there he goes again, right now.
(voiceover): We are learning machines.
Our brains have evolved to be exquisite reward seekers, and that was important for evolutionary survival.
But that came with a price-- our susceptibility to developing addictions.
NARRATOR: Obsessed with that burst of pleasure, the mouse will probe the hole several thousand times over the next hour.
MALENKA: I mean look at this, he's just doing nothing else.
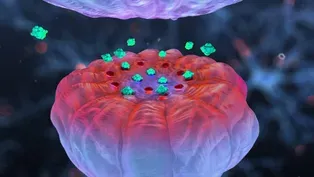
NARRATOR: This experiment revealed the reward pathway in the brain, primarily controlled by a chemical messenger called dopamine.
Dopamine tells your brain to pay attention, that whatever it just experienced is worth getting more of.
It's released by endorphins or when we encounter anything pleasurable or exciting-- especially drugs that can push dopamine levels ten times higher than normal.
MALENKA: All drugs of abuse cause this unnatural rise of dopamine.
And because of that, they're among the most powerful experiences our brains can have.
♪ ♪ NARRATOR: As drugs raise dopamine levels, they also alter the connections between brain cells, creating memoires of euphoria that trigger fierce cravings.
But it's not just about seeking pleasure.
People struggling with addiction soon use drugs to avoid the pain of withdrawal.
JASEN: Withdrawals will make your bones ache.
I couldn't leave the house because I couldn't take a step without soiling myself from the withdrawals.
(shattering) You couldn't talk to me, I'd throw something at you or bite your head off.
NARRATOR: When opioids are abruptly stopped, stress hormones are released at catastrophic levels.
This imbalance triggers the opposite symptoms of opioid use, including shaking, anxiety, pain, and intense dysphoria.
Many times I would lay my head on a pillow and think, "I'm done.
I can't live like this, I don't want to be this person."
And I would wake up the very next day, and I would just do more drugs.
I was powerless over my addiction.
It consumed me, it owned me, I was a slave to it.
♪ ♪ NARRATOR: This cycle of addiction, says Dr. Corey Waller, starts as the brain struggles to rebalance as drugs overwhelm it with dopamine.
WALLER: When that happens, the body decreases the production of dopamine, and eventually you can't even get enough dopamine produced to get out of bed, let alone produce good relationships and good decision-making.
♪ ♪ NARRATOR: To understand what happens to dopamine, Dr. Nora Volkow has been imaging the brains of people with and without addiction to search for changes that occur with drug use.
♪ ♪ VOLKOW: We systematically were investigating individuals addicted to different classes of drugs, and we found that a common change across all of the different types of drug addictions was a reduction in the levels of dopamine D2 receptors.
NARRATOR: The number of receptor proteins, seen here as red in the brains of control subjects, are reduced in brains exposed to drugs.
Fewer receptors means the brain is starving for dopamine.
VOLKOW: Drugs interfere with your motivational drive.
So imagine what it means to lose the motivation to do things, to just not have it.
WALLER: And so anytime someone hears the term motivation, they should really supplant that with dopamine.
Because without dopamine, you don't have motivation.
And so, when we look at a person who is in the throes of an addictive disorder, and say, "They just need to motivate!"
We're telling them to somehow magically make dopamine.
(tumblers spinning) NARRATOR: And it's not just drugs-- gambling or eating can also spike dopamine levels and become addictive.
Volkow found that people with morbid obesity also have fewer dopamine receptors.
VOLKOW: Once those receptors are going down, you are going to have a great difficulty in self-regulating the desire not to eat, because cognitively, your brain is fighting.
On the one hand you say, "I, I'm obese, I don't want to eat anymore."
And at the same time, there is intense craving.
And if your brain is not functioning properly, you cannot win the game.
You are going to give in and impulsively and compulsively eat that food.
NARRATOR: And drugs can unleash even stronger cravings.
JASEN: My wife at the time went and seen her sister for nine days, and I spent $21,000 while she was gone... (chuckles sardonically) on pain medicine.
I did lose my job, I didn't care.
Only thing I cared about was that magical date on the calendar when I went back to the doctor.
WALLER: The body has a drive for dopamine, and that craving flips them into survival mode.
If you understand that this is about survival for them, you can understand why they steal $20 out of your wallet, why they hock jewelry from the house.
JASEN: My habits was putting my wife and my daughter in danger.
Finally, she just done what any mother would do, and they left.
♪ ♪ NARRATOR: Jasen attempted suicide after his brother Scott died of an overdose on the outskirts of town.
For Mark Edwards, it was a moment of reckoning with his own addiction.
MARK: I did not want to be that person that was broken.
And I wanted to get help, but every place that I called didn't have beds available.
I felt like that if I didn't do something, that I would end up dead.
♪ ♪ NARRATOR: Another drug is making the epidemic even deadlier, especially in Vancouver, Canada.
The city has become a gateway for illegal fentanyl, made in China.
Normally used for anesthesia, fentanyl is so potent, it's often shipped a few ounces at a time and later mixed with other drugs.
Hidden in innocuous-looking packages, much of China's fentanyl is headed for U.S. markets.
But it's also devastating Vancouver.
FISHER: Fentanyl is a synthetic opiate created in a lab.
It is super toxic.
So you'll get a batch that comes on the street that's a little bit hot.
And on those days, it's like, bam, somebody's going down, bam, somebody's going down, bam!
NARRATOR: Up to 50 times stronger than heroin, an amount of fentanyl equal in size to two grains of salt will kill you.
(siren blaring) Fentanyl's path of destruction is closely monitored in West Virginia by Dr. Rahul Gupta.
Using a digital map, Gupta follows overdoses as they occur.
Circles stand for non-lethal incidents.
Squares indicate fatal ones.
And a spike of deaths in nearby states means fentanyl-tainted drugs may soon show up in West Virginia.
♪ ♪ GUPTA: On one day, we had 26 overdoses reported to us.
It was almost like a communicable disease outbreak.
And here's the scariest part.
We found that of all of those people who overdosed, none-- no one-- was ever admitted into a treatment facility.
(radios squawking) NARRATOR: But many people don't survive at all because opioids, if taken in excess, can quickly shut down breathing.
Hello?
NARRATOR: And because of the potency of fentanyl, the risk of a fatal overdose is high, no matter who you are or where you live.
♪ ♪ MARY WINNEFELD: Jonathan was a wonderful young man.
From a very early age, compassionate, smart, loving.
Our family did go through many moves.
We lived all over this country, overseas.
So that was, I think, tough for Jonathan.
NARRATOR: Jonathan Winnefeld was born into an accomplished family.
His father James rose through the naval ranks to become the Vice Chairman of the Joint Chiefs of Staff in 2011.
By that time, Jonathan was struggling.
JAMES: At one point, he was in five different school districts in six years, which is tough for a kid.
And so what became apparent to us over time was that Jonathan, as great a kid as he was, was suffering from some form of anxiety and depression.
NARRATOR: Unfortunately, Jonathan was misdiagnosed with attention deficit disorder, and prescribed Adderall, a powerful stimulant.
Soon, to unwind at night, he began to drink.
To calm his anxiety, he used Xanax, a mild tranquilizer, and smoked pot.
Then, he experimented with heroin.
MARY: So we got him into counseling, and I did what a normal parent would do.
I took away the Xbox, I took away his phone, I monitored all of his moves.
In retrospect, it was probably the worst thing I could have done for him, because it isolated him even more.
(sirens blaring) JAMES: And, ultimately, he tried to take his own life.
He ended up wrapping his car around a telephone pole.
It was at that point when we realized that we needed to get Jonathan into inpatient treatment or we were going to lose him.
(typing on keyboard) MARY: I went on the internet and searched, and it's overwhelming.
There are so many different places out there.
You don't know who's good, who's bad, who's just trying to make money.
Financially, our insurance covered nothing.
We really tried to find the best treatment possible out there.
But, in America, there's not a lot of support in the mental health and especially in substance abuse.
NARRATOR: The Winnefelds found a center in Connecticut to treat Jonathan's addiction and anxiety.
Like some 80% of programs, it followed the 12-step model of Alcoholics Anonymous, where patients admit they are powerless over drugs, need help from a higher power, and commit to abstinence.
WALLER: If we look at the legacy treatments that've been around for 70 years, they revolve around going to meetings and working through the 12 steps, generally doing that a lot with self-help and group-based therapy, and then maintaining that abstinence by using that alone.
NARRATOR: Jonathan's treatment for 15 months cost the Winnefelds hundreds of thousands of dollars, but it seemed worth it.
JAMES: Our son came back to us.
We were able to have a real conversation with him.
We saw, about a year into his treatment, that he regained his ambition.
♪ ♪ NARRATOR: Seeming confident of his recovery, Jonathan enrolled as a freshman at the University of Denver.
JAMES: That day we dropped him off at his dorm, he was excited, looking good, fired up, and it was one of the best moments of my life, seeing him doing so well.
(phone vibrating) NARRATOR: Three days later, their hopes were shattered.
MARY: I was not prepared to get a phone call saying that my son had passed away in his bed, in his dorm room, from heroin and fentanyl.
Never, never, never would have guessed that in a million years.
♪ ♪ NARRATOR: With failure rates nearing 80% to 90%, is the abstinence-based approach to opioid addiction scientifically flawed?
Abstinence-based programs really, for opioid use disorder, are setting people up to fail and to relapse.
And in the face of this crisis, where we know that every single time that somebody uses an opioid, they are at real risk of overdosing and dying, this should never be recommended as a primary intervention.
NARRATOR: In Morgantown, West Virginia, Dr. James Berry also believed abstinence-based treatment was failing his patients with opioid addiction.
(nurse talking indistinctly) BERRY: We would get them successfully detoxed, get them exposed to family therapy, group therapy, individual therapy, and we'd find that they would invariably relapse, and they'd just be out there on the streets using again.
♪ ♪ NARRATOR: Frustrated, Berry considered using methadone, a long-lasting opioid that curbs cravings from heroin and pain pills without causing euphoria.
Methadone binds to opioid receptors and normalizes brain functions altered by addiction, including dopamine levels.
Here is your medication, sir.
NARRATOR: Under current laws, most patients must take it at clinics.
Here is your medication, sir.
NARRATOR: In 2003, the opioid buprenorphine became available under the brand name Suboxone, which could be taken at home.
Less potent than methadone, Suboxone only partially activates opioid receptors to reduce cravings.
If taken as prescribed and not misused, both drugs cut mortality by about half.
After a year, 40% to 90% of patients are in recovery.
You feeling better?
NARRATOR: Berry began giving patients Suboxone.
Oh, yeah, 100%.
They started doing well, they started getting their lives back, they started getting to work again.
Uh, Lawrence, how are you?
Good.
And how much time do you got today?
I got like 260 or... BERRY: 245 days!
245, okay, yeah.
Tell us what you have been doing the last two weeks.
Work has picked up.
I'm about to buy into my boss's business, yeah 35%.
He's gonna let me buy in.
No kidding!
So that will be awesome for me.
So you've really showed him what you've been able to do.
Yeah, yeah.
The main thing that makes Suboxone so effective is it's helping with these cravings that people are experiencing.
But it's so hard to break that chain.
BERRY: Patient after patient after patient will tell me the same story.
"Listen, Doc, "I am not using to get high anymore.
I am just using not to be sick anymore."
What Suboxone does is it satisfies those cravings in a way that they're under control.
It works so much better on calming that demon inside you.
If I went home, started doing opiates again, I was going to kill myself.
(indistinct talking) NARRATOR: With cravings under control, patients can take advantage of a range of therapies to help them cope and rebuild their lives.
LEMBKE: There are fantastic psychosocial interventions like retraining your brain, being mindful, learning more adaptive coping strategies.
The night before, I was saying... CARRIE WILKINS: Because it's not just one epiphany moment.
It's a learning process.
You have to learn to be sober.
And it takes practice, it takes trial and error.
And you've got to be ready for the ups and downs.
♪ ♪ NARRATOR: One challenge, according to psychologist Rita Goldstein, are the changes that occur with addiction in the brain's executive control center, the prefrontal cortex.
This is the prefrontal cortex, in the front of the brain.
And we're looking at gray matter, separating it from the white matter.
So you can see, it's actually tinted gray in this scan.
♪ ♪ NARRATOR: Scans reveal that chronic drug use is associated with reduced grey matter, especially in the prefrontal cortex.
GOLDSTEIN: Those regions are essential to make advantageous choices-- to make the right decision at the right time.
So, the lower the gray matter, the more the decision-making is impaired.
You have a decrease in the ability to control your behavior.
NARRATOR: Neuroscientist Yasmin Hurd has found another way that chronic drug use impacts the brain.
By analyzing the brains of overdose victims, she's discovered that heroin changes the activity of key genes.
Heroin changes the way our DNA functions.
It turns on genes that should not be on.
And turns off genes that should be on.
And so that imbalance changes the brain function.
♪ ♪ NARRATOR: The genes most affected regulate the brain's key chemical messenger, called glutamate, which is essential for sending signals between neurons, making thinking, memory, and learning possible.
HURD: It's not that addiction completely takes away every aspect of your cognitive function.
In fact, you have to work even harder.
So I think people need to understand that people with these disorders are actually fighting a very strong battle.
NARRATOR: But is this a battle that can be fought and won?
Opioids are still being studied, but scans reveal that dopamine receptors reduced by other addictive drugs can come back with recovery.
Rita Goldstein has seen evidence that grey matter can increase.
The ability of the brain to heal and to recover is amazing.
So definitely there is a lot of hope.
HURD: The question is, "How long does it take?"
And everyone's brain is different.
(siren blaring) NARRATOR: Yet most people don't have access to effective treatment, especially medications for opioid addiction.
♪ ♪ For Dr. Corey Waller, the problem is that addiction is not handled like other diseases.
WALLER: If a patient comes into an emergency department with chest pain, we have a pretty standard set of approaches.
We evaluate whether or not the heart's being injured.
We look at an E.K.G.
that tells me, "Do they need to get something done quickly?"
And no matter what the answer is, we actually have a place for them to go.
NARRATOR: For overdose victims, the focus is mainly on revival.
These are patients who are basically dead.
They're not breathing.
They are this close to being dead forever.
WALLER: Let's give the Narcan real quick.
NARRATOR: The drug naloxone, sold under the brand name Narcan, can reverse an overdose by pulling opioids off receptors in the brain.
You all right?
Good.
WALLER (voiceover): And in most emergency departments around the country, that's the extent of the intervention.
Check the box, sign the chart, discharge the patient.
Unfortunately, we discharge them back out into the wilderness, where there is no consolidated, appropriate care for them.
Big, deep breaths.
NARRATOR: Although Narcan saves lives, it can also put patients into acute withdrawal.
Without medications to control cravings, many will overdose again.
WOMAN: Oh, my God.
(child crying) KEHOE: This human tragedy really is a human rights issue.
The last thing we should be doing is kicking people out of care.
That's when they're in crisis.
♪ ♪ NARRATOR: Massachusetts General Hospital runs one of the few programs in the U.S. that immediately offers overdose patients medications to control cravings.
KEHOE: This is a treatable illness.
We have to have people in that moment who can say, "Hey, I'm here to help you.
"Are you interested in engaging in care?
We have Suboxone we can start you on right away."
We're seeing people come that day and engage in care, and the vast majority of them, 75% to 80%, are returning.
♪ ♪ What's going on here?
Did we tolerate it?
NARRATOR: Since effective treatment is hard to find, the costs of the epidemic continue to rise.
In Charleston, West Virginia, Dr. Stefan Maxwell cares for babies born dependent on drugs.
(baby wailing) MAXWELL: It's a withdrawal syndrome.
They have vomiting, diarrhea.
Frantic behavior, they may scratch themselves.
These babies may go for many days without sleeping or eating.
And symptoms may last up to three months.
NURSE: I know, baby, I know.
NARRATOR: Babies in acute withdrawal are weaned off opioids by giving them smaller and smaller doses.
I just gave her a methadone about five minutes ago.
NARRATOR: Every 25 minutes, somewhere in the U.S., a baby is born dependent on opioids.
Many will become wards of the state.
We have amongst the highest number of foster children in the nation per capita.
We're having difficulty finding parents and providing services.
In fact, we believe it cost over a million dollars per child additionally if they're born dependent on drugs.
♪ ♪ NARRATOR: Many parents with addiction are also facing challenges like poverty and trauma.
BESSEL VAN DER KOLK: Trauma is an experience that overwhelms you, that leaves you bereft, paralyzed, and with no way out.
And it can come in many different contexts.
It can be physical, verbal, sexual abuse, childhood neglect.
And these problems early in life put you at risk later in life.
NARRATOR: Studies show experiencing a combination of five adverse events can increase the risk of addiction tenfold.
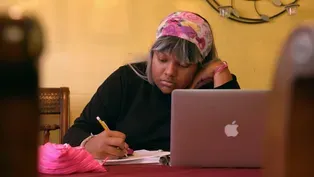
Trauma can cause long-lasting changes in the brain, leaving sufferers like Marie also vulnerable to depression and anxiety.
We had somewhat of a decent family life, you know, but I watched my dad beat my mom my whole life, you know.
My dad was an alcoholic.
They finally divorced, and me and my mom moved out here.
And my mom kind of lost it.
That's when I started really, just, you know, going wild.
VAN DER KOLK: What you're left with as a kid, is these heartbreaking feelings of "I'm no good" and "The world is a terrible place."
Somebody says to you, "Here is something that will make these feelings go away."
And so, people take drugs because they can't stand the way they feel.
NARRATOR: After Marie had her first child, she became addicted to OxyContin.
Child Protective Services took custody of her son until she could pass her drug tests.
For a while, things went well.
But Marie began struggling after giving birth to her second child.
MARIE: I went home to see my first son, you know, because I hadn't been spending time with him.
And then I got a phone call, and CPS said, "Get ready, "'cause we got to meet you in Charleston to take your kids."
NARRATOR: During her pregnancy, Marie had been given methadone for free.
But after her delivery, she had to pay for her treatment.
With no money or insurance, she relapsed.
It's a reality faced by countless people without resources.
MARIE: By that time I owed the methadone clinic over $600 and some, you know.
And, of course, when you go back, you know, they wouldn't see you no more because I owed them too much money.
So I couldn't, I couldn't dose no more, so here I am back at it again, you know.
(sniffles) MARY PRICE: She needed services that were lacking here in rural West Virginia.
She needed those to be available for her, and they're not.
And that saddens me, because... because I know... that the mom's hearts break.
(radio squawking) MARIE: I'll never forget that whole scene in my life.
they surrounded us with cops, and that was not needed, you know.
And my three-year-old said, "Mommy, hold my hat while I'm gone."
(voice breaking): And... they took him away.
WALLER: People always want to talk about, "How do we stop the cycle?"
That's how we stop the cycle.
You don't stop the cycle by pulling the baby because mom took drugs.
We just need to see it and treat it like it's any other disease.
You get the mom stable, you get baby stable, and you go home with a family.
♪ ♪ NARRATOR: Back in Vancouver, the opioid epidemic spurred the city to take bold steps, even before fentanyl tainted the drug supply.
In 2003 it sanctioned the first legal site in North America where people could inject illegal drugs under medical supervision.
Called Insite, the program provides clean needles to prevent the spread of infectious diseases, drugs to reverse overdoses, and help accessing services, like medically assisted treatment.
FISHER: When people come to Insite, often the first thing that they're thinking is, "I need a safer place to use.
"I don't want to die in the alley.
"I'm tired of living in, essentially, what are Third World conditions."
So what we're doing is we're saying, "Come on in to First World health care."
And in the years since Insite's opened, overdoses in the area have gone down, and our H.I.V.
rate in Vancouver has plummeted dramatically.
NARRATOR: Insite's success bolstered other efforts.
At the Overdose Prevention Society, Sarah Blythe helps people test their drugs for fentanyl.
But that's not the only contaminant she's worried about.
BLYTHE: Because we've seen everything from cement filler to Comet to pig de-wormer, like, you name it, anything that they can put in there, they do, and it's dangerous.
NARRATOR: A pink stripe indicates the presence of fentanyl.
It's now found in 88% of illegal opioids here.
Like many longtime users, Daniel knows he's injecting fentanyl, but the fear of dying isn't as powerful as his cravings.
He first took opioids in prison to calm his anxiety.
There's always a fear of something horrible about to happen.
There's going to be somebody getting stabbed, a fight's going to break out.
And so when I did that first hit, it was the first time I felt like I could relax and not have to worry.
♪ ♪ FISHER: To my mind, obviously the most important thing about supervised injection sites is that it implicitly says that, "These lives are worth saving, these people are valuable to us."
What's really important about it as well is that it's a space of connection.
That's the space that people are going to ask for help from.
NARRATOR: Supervised injection sites are illegal in the U.S., but in Canada, the controversy is waning.
For 22 years, Bill Spearn has walked the streets of the downtown east side.
Although drugs are still here, overdose deaths decreased 35% after Insite opened.
Once a skeptic of supervised injection sites, today he's not.
SPEARN: Does it increase crime?
Does it encourage drug use?
Is Insite a big magnet that attracts drug users from all over the world?
And the answer is no, it doesn't.
And I think that harm reduction is something that every city should consider, because it keeps people alive.
FISHER: It actually saves taxpayers dollars.
The most expensive housing that we have in this society?
Emergency rooms and jail cells.
We need to quit putting people in those and start putting people in more compassionate spaces like supervised injection sites.
♪ ♪ NARRATOR: Meanwhile in West Virginia, heath commissioner Dr. Rahul Gupta, is also trying to reverse the soaring number of overdose deaths.
Today he's traveling with a volunteer medical team to bring free health care to McDowell County and take steps to stop preventable deaths.
GUPTA: This is naloxone.
NARRATOR: Because overdose fatalities here are seven times the national average, Gupta and his colleagues are trying to get naloxone, the overdose reversal drug, to as many people as possible.
That's how this drug works to save your life, okay?
But after that you've got to get help as well.
I don't look at this as a single epidemic.
I look at this as multiple epidemics coming together and evolving in real time.
NARRATOR: Gupta is worried about the huge spike in hepatitis and the rising number of H.I.V.
cases.
Patients are offered free testing to see if they need treatment.
VOLUNTEER: It just takes 20 minutes.
Now, I also want to talk to you about a needle exchange, are you okay with that?
Okay.
NARRATOR: McDowell is one of the few counties that allows needles to be handed out to prevent infections.
Okay?
The idea here is to have your own set.
NARRATOR: According to Gupta's analysis, every dollar spent on harm reduction saves up to seven dollars in medical costs and steers people towards treatment.
...when you do want to get help, whether it's counseling or any other aspect, we're here to help you.
♪ ♪ The cost are really unsustainable if we continue this path, losing over half a trillion dollars a year for multiple years in our economy.
We've got to be smart about addressing addiction.
We have to find ways to prevent it from happening in the first place.
VOLKOW: As a country, we have neglected it, and we have stigmatized it, and we have criminalized it, and that has not solved the problem.
In fact, it has made it worse.
NARRATOR: But America's addiction crisis is not just limited to opioids.
Each year over 80,000 people die from excessive drinking.
Smoking is responsible for over 400,000 deaths.
And so if we don't build a stabilized, appropriate, evidenced-based treatment system for addiction, then the reason that medicine gets so costly every year is because what we're trying to do is not intervene on the front end, we're trying to fix everything that's broken on the back end.
The solution to this is for us to embrace addiction as a disease, to bring it within the house of medicine, so that anybody struggling with addiction can walk into an emergency room, or a pediatrician's office, say, "I'm having a problem with drugs or alcohol, will you help me?"
And that the answer is an enthusiastic "Yes!"
(turn signal ticking) NARRATOR: Today most people struggling with opioid addictions cannot access medications or treatments proven to be effective.
Some people recover on their own, but it's rare.
Jasen is one who beat the odds.
He is remarried and delivers cars for his brother Mark's business.
♪ ♪ JASEN: I am not the man that I want to be, but I'm not the man I used to be, thank God.
I try to become better every day.
Sometimes I fail, sometimes I succeed.
But I keep trying.
(cooing) NARRATOR: Mark recovered after five years of methadone treatment, followed by a faith-based program.
MARK: And that love began to change me in a way that I didn't think would ever be possible.
Shoot!
Oh, good shot!
NARRATOR: Casey is now on Suboxone and studying to become a doctor.
Her muscle cramps have been diagnosed as fibromyalgia and rheumatoid arthritis.
To control her symptoms, she takes 11 other medications, but none are opioids.
Happy... (voiceover): Recovery is definitely possible.
It might take years or months or however long, but it is possible.
♪ ♪ NARRATOR: Marie is on Suboxone and getting group therapy, paid for by Medicaid.
Today, she is going to see her youngest son, who lives with a foster family.
Bubby, come here.
What are you doing?
Get me in!
Come here and give me a hug, Booga!
Mmm, I love you.
(voiceover): That baby means so much to me.
Now that I'm getting it together, I hope that as time goes by, they'll see a difference in me, you know.
NARRATOR: As long as Marie is in recovery, she can visit her children.
Ready?
I want to go with you.
I wish you could go with me, Bubby.
I want you to go with me, if you only knew.
If you only knew.
FISHER: People recover from addiction.
They need basic stability, stability of relationships, they need housing, they need that sense of a future that they can look forward to.
When we offer people things like that, they get better.
They are better.
Nobody is unreclaimable.
♪ ♪ Major funding for "NOVA" is provided by the following: NARRATOR: The Concorde.
A triumph of technology.
MAN: An airplane that can still outperform most air force jets.
NARRATOR: Cruising at twice the speed of sound.
(cork pops, bubbles fizz) The ultimate in luxury.
Until tragedy struck.
Are we ready for a new generation of supersonic flight?
MAN: This is going to change the way all of us get around the planet.
NARRATOR: "Flying Supersonic," next time on "NOVA."
♪ ♪ To order this "NOVA" program on DVD, visit ShopPBS or call 1-800-PLAY-PBS.
This program is also available on Amazon Prime Video.
♪ ♪
Video has Closed Captions
Discover how opioid addiction affects the brain and how treatments are saving lives. (1m 54s)
Canada’s Bold Steps to Reduce Opioid Overdoses
Video has Closed Captions
Vancouver, Canada’s supervised injection sites offer people a safer place to use. (6m 3s)
A Coal Miner's Story of Addiction and Recovery
Video has Closed Captions
After a mining accident, a West Virginia resident began struggling with addiction. (3m 36s)
Former Opioid User Discusses Withdrawal and Recovery
Video has Closed Captions
Ben Francis became addicted to opioid painkillers in high school after a soccer injury. (2m 30s)
Helping Children Born Dependent on Opioids
Video has Closed Captions
A therapy program enables children born with neonatal abstinence syndrome to build skills. (3m 44s)
How a Teenager's Opioid Prescription Led to Dependence
Video has Closed Captions
Severe muscle cramps landed this teen in the hospital, where she was prescribed opioids. (3m 57s)
The Science of Opioid Addiction and Treatment
Video has Closed Captions
How opioids mimic the body's natural pain relievers and sometimes induce euphoria. (3m 8s)
Why Addiction Stigma Stops Patients from Seeking Treatment
Video has Closed Captions
Over 20 million Americans struggle with addiction—and social stigma is partially to blame. (1m 57s)
Providing Support for PBS.org
Learn Moreabout PBS online sponsorshipNational corporate funding for NOVA is provided by Draper. Major funding for NOVA is provided by the David H. Koch Fund for Science, the Corporation for Public Broadcasting and PBS...